How Gut Health and the Immune System Affect Your Brain
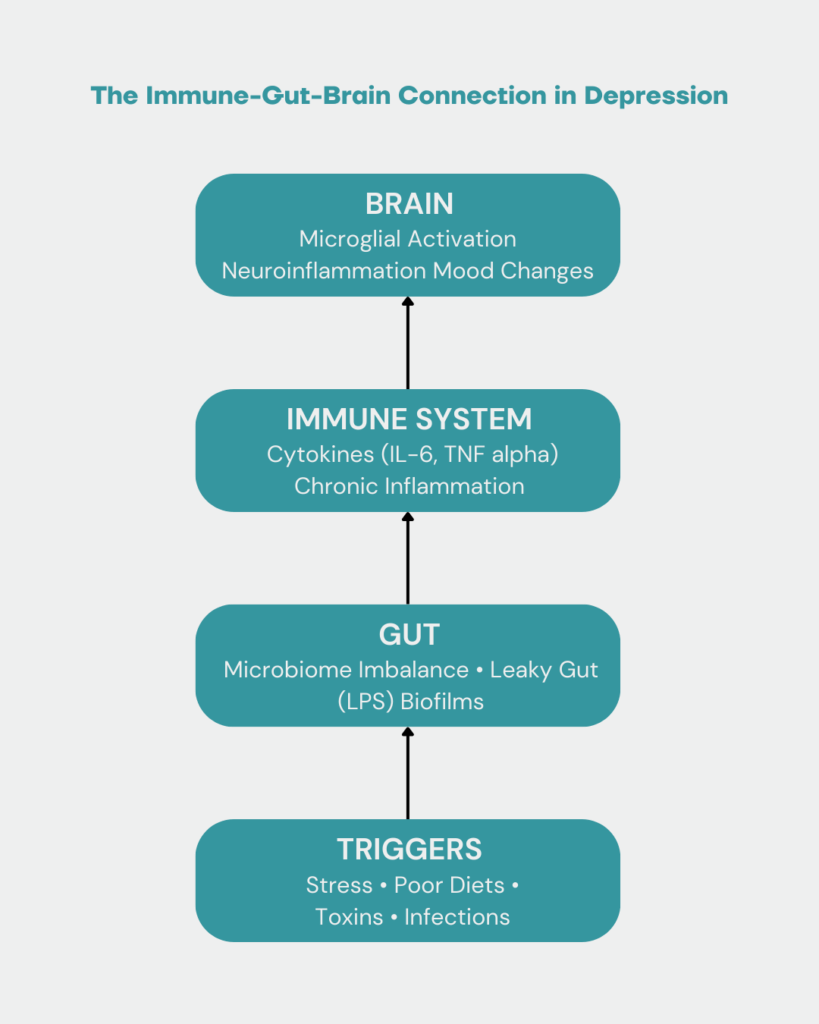
For years, depression has been explained as a “chemical imbalance” — especially low serotonin, the so-called happy chemical. That’s why antidepressants are often prescribed to restore balance. But new research shows there’s much more to the story. While neurotransmitters like serotonin, dopamine, and norepinephrine are important, they are only part of the puzzle. A hidden driver of depression is neuroinflammation — inflammation in the brain — which is strongly influenced by gut health and the immune system.
The Role of the Immune System in Brain Health
Your immune system is designed to protect you from bacteria, viruses, toxins, and injuries. When it senses a threat, it sends out cytokines, chemical messengers that spark inflammation.
Short-term, this process is helpful. But when inflammation becomes chronic (lasting months or years), it can damage the brain’s delicate balance.
Normally, your brain is protected by the blood–brain barrier (BBB) — like a security fence. But chronic stress, poor diet, toxins, or infections can weaken this barrier, allowing harmful immune chemicals to slip into the brain.
Once inside, they activate microglia — the brain’s immune defenders.
Microglia: The Brain’s Immune Cells
Microglia are like the first responders of your brain. They protect against infections and help repair damage. But if they remain switched “on” for too long, they can begin harming healthy brain cells.
This can:
-
Disrupt neurotransmitter balance
-
Slow down new brain cell growth (neurogenesis)
-
Interfere with communication between brain cells (synaptic plasticity)
The outcome? Symptoms such as brain fog, fatigue, low motivation, and depression.
Gut Health and the Immune System: The Missing Link
One of the biggest sources of chronic inflammation comes from poor gut health. Here’s how it works:
-
The gut microbiome becomes unbalanced — harmful bacteria outnumber the beneficial ones.
-
Harmful microbes release toxins like lipopolysaccharide (LPS).
-
These toxins damage the gut lining, creating a “leaky gut.”
-
Undigested food particles and toxins leak into the bloodstream.
-
The immune system reacts, inflammation rises, and signals reach the brain.
-
Microglia become activated, sparking neuroinflammation.
This shows why gut health and the immune system are deeply connected to your mood and mental health.
Why Does Gut Health and the Immune System Connection Matter for Depression
Depression isn’t only about brain chemistry. It’s also about what’s happening in your gut and immune system. For many people, addressing hidden sources of inflammation can make a big difference in recovery.
Healing steps often include:
-
Eating an anti-inflammatory diet rich in whole foods
-
Using targeted probiotics to support gut balance
-
Reducing exposure to toxins in food, water, and environment
-
Treating hidden infections that drive inflammation
-
Supporting digestion and detox pathways
By focusing on gut health and the immune system, we can target the root causes of depression instead of just managing symptoms.
Your brain doesn’t work in isolation. It’s connected to your gut and immune system, which means improving gut health and reducing inflammation can have a direct impact on mental health.
At Functional Mind LLC, we look beyond neurotransmitters and help restore balance by addressing neuroinflammation, gut health, and immune function.
How Dr. Achina Stein Can Help
Dr. Achina Stein is a Functional Medicine psychiatrist who specializes in uncovering the root causes of depression and other mental health struggles. By addressing gut health, the immune system, toxins, and inflammation, she helps patients restore balance and resilience.
📞 Call: 401-270-4541
📅 Book your FREE 25-minute discovery call today:
👉 fxnmind.com/free-consultation-with-achina